Please check out my present-day blog:
The Quirky Quad Diaries – www.QuirkyQuad.com
As many of my friends and family know I have arrived safely in Raleigh North Carolina and have been living here for almost a month now.
I have many great and some challenging memories of the last 2 1/2 years in Kunming participating in the walking program and just generally living in China. At the moment I am working towards building a new life here in Raleigh with finding caregivers, getting an apartment set up, meeting new people, etc.
I apologize I’ve not written sooner, but as you can imagine moving a quad across the ocean is quite an undertaking! On my journey across I had my mother and my biggest brother take me 30 hours to get back to the United States. It was quite an interesting experience trying to transfer a quad onto an airplane as many of my handicap friends will understand.
I have to say I’m going through a mild culture shock at the moment being back in the United States, but like with any new situation, it will just take some time to adapt.
I plan on starting a new blog over the next several months in Raleigh on the topic of adventures in Raleigh with a twist of educational information for fellow SCI folks on SCI research, pressure sore care, wheelchair issues, etc. I also found it challenging when researching on websites for SCI that there are not more practical guides on how to do something or deal with a particular situation right away. I have to develop my thoughts further on how to approach this new blog, but I will definitely keep everyone updated through my Facebook. You can find me on Facebook at Ali Ingersoll. I will also be posting updates for my Facebook account on a regular basis.
CONTACT information: please feel free to e-mail me moving forward at Ali@Ingersoll.org or you can call my cell phone at 919-395-1491 if you have any questions or want to talk about anything with me.
To end this blog I thought I would post a series of photos from my last few days in Kunming where the whole rehabilitation team attended a party we hosted for them at the rehab center, which included a lot of food and even some dancing.
I also spent my last weekend in Kunming going ice skating… Yes you heard me right! There is an ice skating rink on the fifth floor of this very large mall and at first the staff did not want to let me put my wheelchair on the ice and skate or rather be pushed around the ice.
We came to a very interesting compromise where they said I would be able to free skate around the rink with everybody if at first I would be the centerpiece for an ice show. They put me in the middle of the ice rink where I waved and smiled while multiple ice skate dancers skated around me with a whole light show. It was probably the most amusing thing I had done in Kunming since I had arrived other than maybe going to see the little people.
I also have some wonderful videos that I’ve uploaded on Facebook for you to have a look at: https://www.facebook.com/ali.ingersoll/videos_by Please let me know if you cannot view the videos and I will upload them directly to the blog.
Enjoy the photos and I want to thank many of you would’ve been such tremendous support for me since I broke my neck and the last several years over in China. I keep in touch with most of you but those of you who only get information through my blog please feel free to reach out to me anytime.
再见 and goodbye!
QUAD ICE-SKATING
GOODBYE PARTY AT TONGREN HOSPITAL
First off, I would like to apologize for my months of blog silence, as I have recently been focused primarily on getting my trading career on track.
As it turned out, these months have been exceptionally interesting as well as successful, and I now have a clearer and positive picture of the future.
Presently, I am gearing up to move back to the United States at the end of May, when I’ll be relocating to Raleigh, North Carolina to live near my sister, Tiffany. For a quad to move her household anywhere is quite an undertaking, never mind half way round the world, so we’ll really have our hands full over here this spring.
In addition to working full-time in recent months, I have continued to go to the Kunming Tongren hospital every weekday morning for a rehab workout routine that keeps me in shape and generally maintains good health.
Saturday Lunch with Neurosurgery Leaders
Yesterday, Saturday, I was invited to lunch with Dr. Zhu, the head of the Kunming Walking program, and with Dr. Liu, Tongren Hospital’s top neurosurgeon. We drove outside Kunming to Dr. Zhu’s country home for a wonderful traditional Chinese lunch plus a tea-making ceremony + lesson.
Participating in a formal Chinese tea ceremony is a truly fascinating experience that reflects many, many centuries of tea culture. One does not just pour tea into a pot of hot water and then into a cup as in the western world. Instead, tea preparation is elaborate and time consuming, varying significantly according to the type of tea available.
The variables include what type of tea is on offer, how long to steep the tea in a pot, how to prepare the teacups and teapot and finally the temperature at which to drink the tea, with different cup types for different teas. I have included below some pictures from our Saturday outing. There are many online resources, including YouTube videos that set all this out in further detail.
http://en.wikipedia.org/wiki/Tea_ceremony.
When it came my turn to make tea, this turned out to be comical and painful at the same time. For I had to pour the tea with no finger movement, which involved me burning my hand, but I did not want to insult Dr. Zhu, so I decided to say nothing about several burns on my hands. Yikes! 🙂
But the experience was somehow still fun, and the pictures speak for themselves.
Dr. Zhu and Ali
Dr. Liu, Dr. Zhu and Ali
Jenny Emma and Ali
Incredible homemade Chinese spread prepared by Dr. Liu
Sterilization of the teacups
Traditional Chinese Tea Ceremony table
Dr. Zhu’s insane tea room
Cleansing of the teacups
Mom taking the lead in preparing the tea
Attempting solo Tea pouring mission… A painful one!
New Charitable Grant = Astonishing Offer for International SCI Patients
As we were enjoying our delicous Chinese lunch that Dr. Liu had personally prepared, (this hobby showcasing one of his many talents) he and Dr. Zhu informed me of an exciting – even astonishing — new initiative they have just launched.
International SCI patients are now being invited to Kunming for six months to one year to participate in the Kunming Walking Program, free of charge. Yes, you heard me right!
Free of charge for international patients, even including spinal cord surgery if required.
In order to promote the Kunming Walking Program, the Tongren Hospital has been given a charitable grant to invite multiple international SCI patients to join the program free of charge. The only expenses needed to be paid by each patient will be a plane ticket to Kunming and local food.
The hospital will cover accommodation, surgery (if deemed necessary), rehabilitation and participation in the Kunming rehab walking program.
While regular readers of this blog might have reservations about accepting such an offer, given a few of the mishaps I have endured, after two years here I have nonetheless come to the conclusion that a good case can be made for international patients joining the Kunming Walking Program:
Summing up …
I think if an SCI patient joins to this program without unrealistic expectations, then the Kunming SCI program has a tremendous amount to offer.
For example, you may not walk again or even regain other motor function, but rather you can be pretty confident you will increase flexibility, range of motion, build useful muscle mass, significantly improve adaptive behavior (like how I can raise my arms over my head without functioning triceps) and generally get back in better shape.
In this case, with realistic expectations, I think Kunming program is well worth the effort to come here and really give it your best effort.
As for potential need for corrective surgery, Dr. Liu and his team have a well-deserved international reputation for extraordinary competence and experience refined over many years and thousands of patients. They are truly remarkable.
Finally, maybe as an “extra” — there’s the opportunity to learn first-hand about Chinese culture and even to speak the language … well, China is fascinating and just has so much on offer!
All that said, I need also to point out that if a quadriplegic would like to apply to join this program, it would be important to bring over your own caregiver or family member to assist you, because Chinese caregivers, while excellent, do not speak English.
Apropos culture and language, Tongren Hospital does have on its full-time staff a charming Chinese woman (“Emma”) who is fluent in English and who is available to help international patients with translation and generally getting settled into the program. Indeed, that’s her main responsibility.
If you are interested in what is now being offered by Kunming Tongren Hospital, you’re welcome to e-mail me at Ali@Ingersoll.org and I will be happy able to make the introductions to Dr. Zhu Hui as well as to Emma so you can figure out if coming over to Kunming makes sense for you.
Summing up, I think the new grant-supported offer is a once-in-a-lifetime opportunity, both for rehab and surgery. And even if you do not regain any motor function, you’ll still have had an experience you’ll never forget.
Think about it!
I would like to offer my sincere apologies to readers who have been writing me over the last few weeks wondering where I have gone.
Well, I’m still here in Kunming, Yunnan Province, China!
Recently, I have shifted my focus from the Kunming Walking Program to full-time trading 10-to-12 hours a day. “A girl has to make a living!”
🙂
I pretty much use the SCI rehab center at Tongren Hospital as a gym now, working out vigorously 4-to-5 days a week for about 2 1/2 hours each day in order to stay in shape.
I will be slowing down my blog post entries over the coming months as I will be focusing a majority of my time on work. When I do post, I will update my blog with general news and photos of what I’m up to over here in China, and I will also focus on the progressive pain-reduction work I have been doing with my Chicago-based hypnotherapist, Dr. Stephen Kahn.
I have been working with Dr. Kahn for the last 4 months to reduce the intense chronic neuropathic pain that has plagued me for the past couple of years.
Before Steve Kahn’s involvement, I had tried surgical (spinal cord de-tethering) + drug (Lithium carbonate) + physical (acupuncture) solutions to address my pain, but I had no luck with any of these initiatives.
Since pain represents how the brain interprets incoming signals, it stands to reason that I should be able to change how my brain interprets these signals. And hypnotherapy has a clinical history of more than 100 years of being able to deal effectively with a wide range of pain issues.
For readers who may be interested in learning more about clinical hypnotherapy for pain management, I’ll be happy to provide details on a couple of exceptional books that are available in both physical and Kindle format.
I have tried meditation on my own, but I just could not focus by myself, and the meditation recording I was working with was perhaps not personalized enough for my specific needs.
The back story here is that my Dad and a very dear family friend, Ted Hearne, got together in Chicago early last June and interviewed Dr. Kahn, who subsequently agreed to work with me here in China several times a week via Skype video conferencing.
I prefer hypnotherapy, as opposed to meditation, because hypnotherapy provides me with guided visualizations that allow me to focus on specific pain issues. And while every SCI survivor is unique, I have already become a serious advocate of hypnotherapy and guided meditation.
Over the last few months, I would say my pain levels may not necessarily have gone down in an easily quantifiable way, but I’ve learned to refocus my attention, which distracts me from the chronic pain of pins and needles that I experience constantly with varying degrees of intensity.
Many therapies can take a lot of time and effort to produce meaningful results, so I’m minded to be patient with hypnotherapy, as it seems to be working already at some level. I practice every day with my own personal recordings that Dr. Kahn has made for me, and I work with him over video Skype several times a week.
I will keep you updated on my progress, but so far this is the most useful pain management strategy I have found, and I intend to pursue it. Indeed, Dr. Kahn has accepted our invitation to travel to Kunming to work with me face-to-face, and he arrives from Chicago on November 13th for a stay of 10 days.
In heartfelt appreciation …
On a different note, I wanted to take a moment to thank each of my readers for your support over the last two years. I would not have continued writing my blog without your encouragement and comments. Receiving the love and support of friends and family has been absolutely invaluable to my recovery and, yes, continued progress.
Thank You … each and every one of you!
And finally, a special announcement …
In closing today, I have a BIG announcement … I have decided to move back to the United States in April of 2015.
I will be moving to Raleigh, North Carolina and will live just several blocks from my sister, Tiffany, who has resided in Raleigh for the last 10 years. Raleigh (and the greater Research Triangle) is simply a wonderful community populated with exceptionally interesting people.
Tiffany and I have wanted to live nearby one another since we were children, and we have finally decided to take the leap! My sister and I have had the closest imaginable relationship since we were very small. So I’m really extraordinarily fortunate to have my sister as one of my very best friends, and I am so excited to move to Raleigh!
We are starting to organize now with finding an apartment, caregivers, etc. As you can imagine, moving a quadriplegic halfway across the world and getting her installed in her own home is quite an undertaking!
But then … we did it in China … 🙂
Until the next blog, I welcome anyone who wants to stay in constant contact with me to e-mail directly at Ali@Ingersoll.org. I am pretty good at responding to email within 48 hours.
I apologize that it’s been several weeks since my last blog entry, but I’ve been battling with pain issues and also just generally been really busy with work.
A few weeks ago my eldest brother, Colin, came to visit for 10 days. The last time he was here in Kunming was July of 2013, when I was coping miserably with a badly broken leg and pretty much laid up in bed wracked with pain during his entire visit.
So, I was determined during his visit this year to get out and show Colin around the city of Kunming.
Also his visit enabled me to get out myself, because Colin is an exceptionally strong 6ft 4in guy who could lift me over pretty much any obstacle we might encounter in the city.
As you can see below, this blog post comprises mostly pictures from several of our outings.
Perhaps our most unusual excursion was visiting what is known here (and, indeed, throughout China tourism circles) as the Little People’s Kingdom. And I’m not talking about children. Rather, the Little People’s Kingdom is a major tourist attraction build around an actual community of real dwarfs!
The back story here is that a local entrepreneur came up with the idea of advertising all over China for dwarfs who had been marginalized by society. His pitch was to move to Kunming’s temperate climate and live in purpose-built village with lots of other similarly sized people, earning a living by daily live theatrical performances.
Here’s a link to a story run a couple day ago by The Guardian, one of my favorite daily newspapers. Remarkable professional photos here …
The most interesting challenges of our visit included the rough terrain, incredibly steep inclines and raining weather that we had to overcome. I didn’t mind the rain so much because I was in my manual wheelchair and thus knew I would not short-circuit my power chair.
I have to give all the credit to Colin, who pushed me up rocky terrain just to go see the mushroom houses. It was kind of fun confirming that, if I am in the company of a really strong person, I can pretty much travel anywhere in the world despite how non handicap-accessible any particular location maybe.
🙂
Another day, our great friend Jenny Liao insisted we take a gondola/cable car ride up the side of a mountain … remember, we’re in the Himalayan foothills.
Perhaps not surprisingly, Chinese cable cars are about the tiniest things you can imagine!
When I first designed my manual wheelchair before coming to China, I opted to get these little vertical wheels under my wheelchair that would allow me to go down the aisle of an airplane. Thus I was able to pop off my big main wheels and have Jenny and Colin lift me into the gondola car. Honestly, I don’t think we had half an inch to spare, and we had to get in and out several times before we finally succeeded squeezing me inside.
Once we got to the top I was obviously unable to go climbing around the mountain, but the cable car ride was worth it, alone just discovering that I could fit in one with my wheelchair deconstructed.
I am particularly interested in how I fit into cable cars and gondolas because in 2016 I am actually planning a trip to go over to Geneva, Switzerland to visit CERN, the 27 km particle accelerator straddling the borders of Switzerland and France.
While in Switzerland, I intend to be taking as many gondola rides as I can. Maybe I should try to get some sort of skis put on my wheelchair so I could careen down the mountain by myself!
Some of the other photos are just from outings around Kunming, hotels we went to, places we ate, etc. I just wanted to use at least one blog post to show you some of the activities around Kunming in case any readers are thinking about participating in the Kunming Walking Program. Many Chinese agree that Kunming is perhaps the most appealing major city in the country.
I stay indoors at my desk much of the time because I work quite a lot, but there are a great many interesting attractions throughout the city. Indeed, I’m told Kunming is today the #1 national tourist destination for the Chinese.
In my next blog I’m going to devote time to share with readers my progress over the last 3 to 4 months with hypnotherapy dealing with chronic pain. I have been working over Skype video with a hypnotherapist in Chicago and will tell you how this is working out.

Suzanne, Jenny, Ali, Colin, Mom and Dad at an extravagant lunch at the Intercontinental Hotel

Colin and Ali outside the Minority Village

Family Photo at the Intercontinental Hotel

Two little children wanted to take a photo with me instead of the little people at the little people kingdom… I suppose white quadriplegic foreigner is more of an attraction 🙂


Sitting in the rain taking selfie’s before the little People Kingdom performance!

Group photo with the Little people royal guards


Spectacular views from the mountainous countryside where the Little People reside…. And my brother trying to see if I could fly down the hill!

Ali with a little person… Not a child. She is actually in her 20’s


Jenny and Colin pushing me up the incredibly Rocky Hill to go see the mushroom houses
Mushroom houses galore!

Preparation for entering the cable car … wheels off
View from the Chinese cable car looking out onto Kunming city
Inside the cable car
Jenny and Ali at the top of the mountain
My Dad and Colin enjoying lunch in our garden
Sibling love
First a Little Background
Regular readers will be aware that besides breaking my neck in August 2010, I’ve been contending with the further misfortune of being one of those SCI survivors (estimated at 15%) who suffer severe chronic neuropathic pain + debilitating allodynia that is related to my damaged Central Nervous System.
And then there are other pain issues that I share with the broader SCI population, who suffer recurring injuries due to overuse of arms and various kinds of rehab.
For example, I suffer intermittently from an intense a knife-like feeling that cuts directly into my right scapula and shoulder blade where many muscles overlap under the scapula bone.
This pain dates back to shortly after I broke my neck and resulted from constantly driving my power wheelchair with my right arm in a fixed position. Also, rehab weightlifting often aggravates this injury, and it flares up every few months for about 1 to 2 weeks. During break-out episodes, I can barely even drive my wheelchair or exercise.
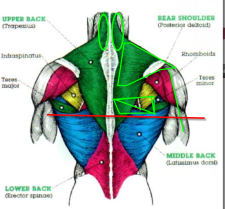
This is a pretty common problem for SCI survivors, who suffer periodically from upper body muscle/tissue damage resulting from life in a wheelchair. And therefore this is why I’m planning to devote a number of upcoming blog posts to sharing with the SCI community what I’m learning about pain management.
So far I have tried quite a few different therapies that have not worked out as I had hoped, but SCI readers may have some luck with these:
In January I also experimented with Lithium carbonate but ended up poisoning myself. By now, though, I’m ready to try another experiment, this time with Traditional Chinese Medicine (“TCM”).
A Brief Overview of Acupuncture
The practice of acupuncture originated in China and has been clearly recorded for over 2000 years. Many different forms of the practice evolved over the centuries and in some cases combined traditional needle therapy along with use of Chinese herbs.
TCM holds that the human body contains a network of energy pathways through which vital energy (called Qi and pronounced “chi”) circulates. These pathways are often commonly referred to as “meridians.”
http://en.wikipedia.org/wiki/Qi
Along these meridians there are specific points that function somewhat like gates through which chi flows as it circulates throughout the body. Acupuncture needles are inserted into these points to free up the flow of chi through the meridians.
TCM further holds that fundamental illness and related symptoms are caused by problems in circulation of chi through the meridians.
Western science has determined that these meridians and specific acupuncture points identified by TCM actually do coincide with anatomical features that can be observed.
For example, electrically-charged particles called “ions” had been found to flow through “ionic streambeds” that correspond with meridians just beneath the surface of the skin. And acupuncture points identified centuries ago by TCM have been found to emit light, which can be detected with sensitive laboratory equipment. How about that for a mind-blowing discovery?
Needle Knife Acupuncture
Needle-knife acupuncture (that’s a literal translation of the Chinese characters) is a special type of acupuncture in which the needles used are very thick with sharpened tips that look like small knives. Here’s what they look like:
In China, needle-knife acupuncture is frequently used to treat knee osteoarthritis.
Then just a few years ago it was discovered that needle-knife therapy was also extremely useful on soft tissue injuries and could help to relieve neurovascular compression by relaxing soft tissues in order to relieve tension pain.
Over the last 10 years multiple universities in China have undertaken large scale needle-knife therapy acupuncture studies, enrolling over 2000 patients who were treated for various soft tissue ailments. It was found that needle-knife therapy apparently had an effective rate of approximately 85% effective rate.
And even the U.S. NIH has published an evaluation paper on the subject … see:
http://www.ncbi.nlm.nih.gov/pubmed/16739840
I have to acknowledge that these large, knife-like needles look scarier than traditional acupuncture needles, but a couple of months ago my Dad and Jenny attended a physician-training session at a Kunming university that offered free treatment to members of the public. Of the 15 or so procedures they witnessed, not one patient seemed even to winch when the needles were inserted … typically shallow at a flat angle.
Unlike traditional acupuncture, needle-knife acupuncture only takes between 3 to 5 minutes per session. Also, depending on the ailment, one only needs treatment 1 to 2 times a week for about 4 to 6 weeks.
I have been told by the Chengdu-based national director of research on this procedure that I will know if I have any relief after the first two sessions.
So, wish me luck as I try this TCM therapy … yet one more experiment on Lab Rat Ali … hoping to discover a path to alleviate at least one type of pain from which I know the majority of spinal cord injury patients also suffer.And even if this doesn’t work … well … I will just keep trying new things until something does work!
Otherwise …
The last few weeks here in Kunming have been pretty hectic as we’ve had an influx of foreign patients coming either to check out the Kunming walking program or researching spinal surgery options.
There’s one lovely Australian family presently here whose son underwent spinal cord surgery last Wednesday to remove a bent screw (!) as well as to remove a large cyst like the one I had last year, and he is currently recovering well. Fortunately, the Tongren Hospital team have gotten the hang of post-surgical pain management.
I’ve also been extremely busy with trading over the last few months. I have a pretty steady routine now, one in which I go to the gym in the morning for 3 ½ hours to work out and then I come back to my apartment for an early lunch. Right after lunch I hit the financial market screens and focus on trading for the rest of the afternoon.
My neuropathic pain has pretty much remained constant, but as I mentioned in previous blogs, I have recently started working with a gifted hypnotherapist, Dr. Stephen Kahn from Chicago. We get together over Skype video several times a week. This subject is more complex than meets the eye initially, but I believe hypnotherapy holds great promise and feel very lucky to be working with Dr. Kahn.
Summing Up
In recent blog posts I have gone into considerable detail about various aspects of my experience in China — this because readers have repeatedly asked me for as much detail as possible.
Today I’m going to offer less detail-oriented readers a summing up of my 18-month experience here in Kunming.
Successful Surgery
Without the spinal cord surgery on offer in Kunming, it seems likely that I would have by now been ventilator-dependent … or dead.
The ascending, rapidly-growing cyst inside my spinal cord was successfully removed in May 2013 at Tongren Hospital by chief neurosurgeon Dr. Liu Yansheng.
While the post-surgical pain management protocol used with me proved to be woefully inadequate, more recent Tongren patients confirm this serious problem has subsequently been corrected.
The Kunming SCI Rehab Program
It is possible to have mixed feelings about the so-called Kunming Walking Program, because expectations figure so importantly into anyone’s feelings.
I have seen no evidence that the Kunming SCI rehab program results in neurological motor function recovery in chronic SCI patients.
On the other hand, I have seen evidence that the Kunming SCI rehab program builds muscle mass and strength for even chronic patients who work hard at the program.
Improved muscle mass and tone, in turn, frequently lead to enhanced adaptive behavior that can mimic neurological recovery. I’ve treated this subject at considerable length in an earlier post, but for now let’s just sum up by noting that improvements in adaptive behaviour, while very useful to SCI survivors, are often mistakenly confused with motor function recovery.
On the other hand, here in Kunming I have quite frequently witnessed functional improvements with acute SCI patients. This may be on account of adaptive behavior or neurological recovery or some combination of the two. It is obviously impossible to assess how these acute patients would have recovered without the local rehab program.
Life in Kunming
Putting medical challenges to one side, life in Kunming has been very agreeable. And this is not just because of the delightful climate, rather also because the Chinese people here are just so genuinely nice.
My care-giving team (sisters-in-law in their late 30s from the Yunnan countryside) are wonderful to me, with qualities too numerous to recite in such a summary. Indeed, Shao-Lin and Shao-Yin are a major reason I’m still living here.
Yunnan Province is renowned both within China and internationally for the quality and variety of its “old China” tourist attractions, and our periodic overseas visitors have really enjoyed the regional tours we’ve organised for them.
My Pain Issues
Regular readers know that I have been greatly troubled by persistent high levels of neuropathic pain as well as allodynia, both of which pre-date my arrival in Kunming.
The more recent neck and right shoulder pain resulted from my surgery here. We now believe this was a knowable risk of which we had not been informed and that it resulted from stretching the intersection where the dorsal root ganglia (sensory) nerves enter the spinal cord. Expert international neurosurgical advice is that this pain may resolve itself over 1-3 years, but I do not see much evidence of that.
With respect to my debilitating neuropathic pain, my Dad has devoted much of the past year to getting up to speed with the neuroscience of pain. He joined the International Association for the Study of Pain (http://www.iasp-pain.org) and has relentlessly pursued both academic and clinical leads all over the globe.
We decided against the use of pain-killing (but mind-dulling) drugs except for very occasional one-time use of Tramadol.
And we concluded that the case for implanted electronic pain management devices has yet to be proven for SCI-related neuropathic pain.
What we have decided to focus on is hypnotherapy. The objective, over time, is to alter what we reckon to be my brain’s pain map, being similar that what is believed to result in the phenomenon known as “phantom pain syndrome.”
And I have already started to work with a renowned Chicago-based hypnotherapist, Dr. Stephen Kahn, former President of the Society for Clinical and Experimental Hypnosis (www.sceh.us).
Readers who may be interested in this subject would find helpful a small book entitled “Medical Hypnosis Primer – Clinical and Research Evidence” that is available from Amazon and offers an up-to-date, succinct overview of the field.
I am already benefitting from working with Dr. Kahn, even as I accept that it will take some while for us to bring my pain levels down on a consistent basis.
Conclusion
The surgical outcome speaks for itself. My ascending spinal cord cyst was already impacting my breathing by the time I came to China, where neurosurgeons have more hands-on experience opening spinal cords than anywhere else in the world. Today my breathing is fine again. So I can recommend Dr. Liu and his team.
My position on the Kunming Walking Program is that its potential value to an international SCI patient depends on expectations. For that reason, among others, I am neither an advocate nor an opponent of the program. As usual “the devil is in the details” … and for details readers will have to comb back through my earlier posts.
On balance, the Kunming experience has worked out well enough for me, notwithstanding my broken leg, chronic post surgical neck pain due to surgery and a few other unanticipated challenges! I suppose those are challenges to consider in and of themselves. And while vexing pain issues still impair my life quality, the neuropathic pain did not originate in China. I will note that living in China has been more manageable for me because I am able to speak the language, which helps with everyday life here in Kunming.
In my blogs moving forward I will be focusing on educational aspects of spinal cord injury, hypnosis, Nerve transplants, etc.
It is been well over a year since I have taken more than a day off from the Kunming SCI program … that is, taking off time from rehab just for fun and not solely on account of pain or other medical issues.
So last week I decided to play hooky from the rehab program on account of my sister, Tiffany, having come all the way from Raleigh, North Carolina to visit me.
Jenny Liao, our trusted Kunming administrative assistant and now very good friend, made us a happy threesome.
So Tiffany, Jenny and I headed out into center city Kunming to do some shopping, have lunch together and to go explore generally.
Most of the pictures that accompany this post are pretty self-explanatory, but we did find our way in several little novelty shops with “Chinese characteristics” as the popular saying goes!
And, as you can see, we even discovered a local branch of the American Toys R’ Us. Great move on their part, as the Chinese are equally crazy about toys and about spoiling their really adorable children.
When we entered the big Toys R Us, you could see right away the sales staff were wondering what on earth we were doing there. Well, in short, we’d come to play!
🙂
When my sister comes to visit, it seems we always revert back to our teenage selves. Why not? Beats current reality by miles!


Sisterly Love
Chinese Shopping Plaza
Right in the middle of a shopping mall!
Boys will be boys? Well, girls will be girls …


Never too old to play Spiderman!

Jenny and Tiffany at “hide and seek”
Hehe … I couldn’t resist!
Middle of a shopping mall is a huge pool with goldfish.
… Where adults + children can go fishing!
Changing Topics … Fear of Dentists!
I mentioned in one of my previous blogs that a porcelain tooth inlay had fallen out about a month ago, and a local dentist actually came to my apartment to glue it back in … twice!
You really get one-on-one service here in Kunming, and my dentist even came over with his assistant late one night when I was in bed to help me out after the inlay came out a second time. I doubt you would find dental service like that anywhere else in the world.
Anyway, my dentist convinced me that it would be best to replace the inlay with a stronger traditional crown. I struggled for days with this decision, because I am quite terrified of going to the dentist and had never had a crown before.
Indeed, I am so terrified of any dentist that when I did decide to go ahead with the crown I had my sister hold my hand the whole time and sing me songs. No, I’m not kidding!

Home Dental Service
(Daytime Session)
Again … at night in bed!
All Smiles in Dental Office
I know this is hard to believe, but I think I was less scared going into spinal surgery last year than I was over getting a crown fitted last week.
Cool as a cucumber I was when rolled into the Tongren Hospital operating room for my spinal cord surgery, but I had to take a pain killer (Tramadol) in order to feel slightly loopy to go to the dentist last week. I guess there’s something about that drilling sound in my head that rattles me psychologically every time.
Anyway, actually getting into the dentist and transferred into the dental chair was quite a challenge on its own right, even with Tiffany + Jenny + Shao-Lin + Shao-Yin all skillfully assisting.
We had to overcome multiple steps, narrow doorways and then there was the hurdle of actually transferring me into the dentist’s chair. As there were no lower side rails on the chair, we even had to tie my legs together so I didn’t fall out.
🙂
My young dentist is very skilled … quite a superstar in my book. What I did find rather hilarious was that at the end of the dentist’s ground floor office there is a huge glass window, so when I transferred into the dental chair passersby outside on the sidewalk could walk up to the glass and watch the procedure!
China … no problem … everyone’s very curious about many things!
Okay … that’s it for today.
Looking Ahead …
I’ll take the next few weeks to sum up thoughtfully the multiple Kunming Walking Program blogs I have written over the past two months in order to offer to prospective international participants the clearest possible picture based on my personal experience here.
Going forward, I am thinking about shifting my blog focus to be primarily educational and informative with respect to a wide range of SCI issues and challenges that I, in addition to many other SCI survivors, deal with on a regular basis.
I regularly receive e-mails from blog readers who have been reporting that from my blog they are frequently learning new things about spinal cord injury and suggesting they would welcome anything further I think would be of community interest.
So, while I may still do personal blog posts from time to time to keep you up-to-date with what’s going on with me in China, I hope to have a general practical focus on making this blog a useful SCI educational site.
If readers have any comments or particular suggestions on other issues I should focus on, please feel free to e-mail me directly (ali@ingersoll.org) or via my blog.
Cheers!
As many of my regular readers will recall, last year I developed very serious post-surgical chronic neck pain that extends from the base of my neck, across my right shoulder, down my right arm and clear through to the fingers of my right hand.
The pain in my right shoulder and arm feels like a sharp steak knife cutting into my flesh and varies between simply painful to being so intense at times that I have to go to bed in the middle of the day to try to get my mind off the pain.
Chronic post-surgical pain was for me a wholly unanticipated outcome, so we’ve given a lot of thought to possible explanations and to whether or not there might be some way of correcting the problem.
Initially, we thought that scar tissue on peripheral nerves nearby the surgery incision area might have formed and be pushing against several major nerves in the vicinity of where these major nerve bundles enter the spinal cord. Descriptions of compressed nerves sound to me quite similar to what I’ve been experiencing.
For many months I was needlessly further distressed because the neurosurgeons at Tongren Hospital here in Kunming insisted that what I was experiencing was not a normal consequence of their work, and they could not offer any possible explanation for what had obviously happened to me.
So at the end of last year, my Dad switched his neuroscience research focus from primarily regenerative medicine to pain management research and clinical options for me.
Over the last few weeks Dad has again been traveling to different countries in Europe and North America and has interviewed highly experienced neurosurgeons, with special thanks to the world-class neurosurgical team at Indiana University.
As it turns out, Dad has learned that acute post-surgical peripheral nerve pain is not as uncommon as we had originally thought.
Plainly there are always risks when opening up the spinal cord, and experienced neurosurgeons advise against any kind of cord surgery unless absolutely essential – this because operating on the spinal cord frequently results in “unintended consequences” … no kidding!
A common enough result of operating on the actual spinal cord, as opposed to just repairing vertebral bone damage, is that nerve tissue gets stretched at the intersection where major peripheral sensory nerves enter the central nervous system.
How’s This Work?
Certain readers may be interested in how major peripheral sensory nerve bundles enter and get spliced into the spinal cord … and how any type of spinal surgery can affect these spinal nerves on a permanent basis, sometimes leaving the patient in chronic pain for years.
From the diagram below you can see there are two blue tube-like structures that enter the spinal cord on the left and right … these are called the dorsal root ganglia. The dorsal root ganglia feed mostly sensory nerve roots/fibers directly into the spinal cord.
On the diagram I have circled in green the area where I had my laminectomy, which means cutting away vertebral bone to access the spinal cord.
In my case, entering the cord was necessary to remove large fluid-filled cysts (circled in red) that were growing quickly and ascending into areas above my original C-6 injury to choke off nerve control of my breathing.
Performing a laminectomy and then cutting open the Dura Mater to gain direct access to the ventral (front) side of the spinal canal has clear potential to stretch the nerve fibers inside the spinal cord.
This is because the cord itself has to be pushed hard over to one side to enable access to a ventral cyst when the surgeon has entered the spinal column from behind.
The problem with this is that once a patient has been “sewn” back up, some of the spinal nerves remain stretched and do not return in their original positions.
Another view of how the spinal nerves enter the spinal cord through the dorsal root ganglion
As some readers may be able to imagine, stretching major peripheral sensory nerve tracts where they splice the spinal cord risks serious consequences for the patient.
It is quite common that this stretching of sensory nerves can result severe post-surgical nerve pain, as has happened to me. Some patients report a reduction in the intensity of pain over the course of a year or two, but it’s not yet clear to me if the throbbing pain ever quite goes away. But that’s my hope … that over time the stretched nerves will reposition themselves.
As for pain levels, I would say my neck/shoulder pain varied between 8 and 9 every single day for the first eight months after surgery in May 2013, and today, a year later, pain levels have receded a little, back to a 7 or 8 depending on my sitting position.
For instance, it is much more comfortable for me to sit in my power wheelchair because I can recline the back rest as opposed to my manual chair that sits me in a constant upright position, causing pretty constant agony.
An illustration of the complex pathways of Spinal Nerves
A global picture of how the dorsal root ganglion fits into the spinal vertebrae
Once I learned from Dad’s recent investigations the likely reason for my chronic neck pain, somehow this helped me in dealing with the issue, because in my particular situation the operation that resulted in the neck pain was absolutely essential for survival.
Indeed, by the time of my surgery a year ago here in Kunming, I was already having serious trouble breathing, so surgery for me was life-critical.
I just wish the Kunming surgeons had been more forthcoming and alerted me to the potential side effect of severe post-surgical neck pain so I did not spend so many months after surgery thinking I was losing my mind.
In all these circumstances, I do accept the risks and “unintended consequences” that always come along with spinal surgery. Frankly, though, I find it extremely hard to accept that my surgeons told me point-blank and repeatedly that they had never ever before had any patient report the kind of pain I had complained about for so many months.
This may be due to the cultural differences in pain culture that
was discussed briefly in a prior blog post. Maybe so.
Post-Laminectomy Syndrome
However, a few months ago I met in Kunming a Sri Lankan patient who is paraplegic, and he, too, had come here for spinal cord surgery to remove multiple cysts in his spinal cord canal.
This fellow is today back home in Sri Lanka, but I’ve learned he has been repeatedly calling Tongren Hospital to complain about chronic thoracic pain that is so debilitating he can no longer work.
There is an actual name for this pain issue. It’s called “Post-Laminectomy Syndrome.”
The bottom line is that spinal surgery is sometimes essential for survival, but the risks need to be made known to the patient before surgery and critically evaluated.
It is reported that as many as 75% of spinal cord injury patients end up with some type of spinal cyst of varying size. This results from internal cord scar tissue impeding the free circulation of Cerebral Spinal Fluid (“CSF”).
However, I have concluded that unless the cyst is actually affecting motor function or critical organs, then I would think twice about having a cyst removed.
From bitter experience, I can tell you that having severe chronic neck pain and barely being able to sit up in a manual wheelchair is another challenge that could and should be avoided by spinal cord injury survivors who do not absolutely need to have this surgery.
Looking Ahead + Summing Up
In my next blog post, I will sum up the last dozen posts on the Kunming spinal cord injury program – this for the particular benefit of fellow spinal cord injury survivors who may be thinking about travelling to Kunming, either for surgery or to participate in the Kunming Walking Program.
Disclaimer:
I’m going to be discussing my post-operative spinal surgery care today, and while this is not for the faint of heart, in response to readers’ persistent questions I’m relating what actually happened.
In fairness, since my surgery several other foreign patients have undergone spinal surgery at the Tongren Hospital, and the staff here seem to have learned from my experience, significantly improving post-operative pain management protocols.
Firstly, I think it may be important to set the stage by discussing the “culture of pain” in terms of East versus the West.
In developed Western developed, complaining about pain is practically encouraged, as this seems to offer pharmaceutical companies many opportunities to produce drugs to address a great variety of types of pain.
When people are in acute pain, as in post-surgery, there are many pharmaceutical options to alleviate the pain, at least short term, and it is pretty standard practice to work with a pain specialist before and after surgery to create a post-surgery pain plan.
In contrast with this perspective, the situation in China is quite different. In China, especially for the generation who lived through the Cultural Revolution 40 years ago, acknowledging pain is considered a sign of weakness, and pain is generally not discussed with medical staff.
I have spoken directly with many Chinese about the concept of pain, and the younger generation definitely vocalizes pain issues more freely. On the other hand, the older generation, including my neurosurgeons, grew up in an era when you pretty much kept perception of pain to yourself, and their answers to my questions reflect this stoic mindset.
I am sure there have been many thousands of Chinese SCI patients before me who underwent spinal cord surgery and experienced intense acute pain afterwards, but out of respect for their doctors they did not complain about their pain, and thus the doctors seem not to have developed an appreciation of the issue.
In the West it is pretty standard to question your doctor and his or her methods as well as to independently research your particular ailment. In China, by way of contrast, this is not the “norm” and as a general rule patients blindly trust their doctors, and especially their surgeons.
Our (Flawed) Pre-Surgery Due Diligence
In advance of my surgery my brother Mattias and Dad did question my surgical team about post surgical pain management and were assured that pain drugs would be administered.
Thereafter most of the discussion focused on my neurosurgical team’s pride in having recruited the just-retired head of anesthesiology of Kunming Medical School to personally manage on my surgical anesthesia. Thankfully, there were no issues with the general anesthesia.
I do take some responsibility for what I’m about to describe because I assumed by post-operative care they intended to use either morphine or Fentanyl — a synthetic 3x stronger than morphine.
Oh boy, did I ever come to regret not doing a little bit more research on pain management protocols here at Tongren Hospital before the surgery and, specifically, for not having asked what drugs they planned to use on me.
Bound + Gagged …
After successful surgery I was wheeled into the ICU where my family was told that they would not be allowed to visit me for the next 24 hours because I needed to rest.
Well …
I woke up in the ICU and immediately started feeling like somebody was slicing open my spinal cord as if they had not finished the surgery. Unfortunately, no one had told me that when I woke up from surgery I would still be intubated — meaning the anesthesia breathing tube had been intentionally left inserted down my throat. Needless to say, I was unable to speak, being only able to moan and cry from the savage severity of my pain.
My hands flailed frantically in the air as I tried screaming through the intubation tube, while hitting doctors and nurses left and right to signal to them that I needed to speak. I did not think they had properly sewn up my neck as the pain was like nothing I had ever felt before.
I don’t know how many minutes or even hours passed of me moaning and hitting people, but finally the staff took some sort of purple string and literally tied my wrists to the railings of the bed. I remember this vividly, as if it had happened only yesterday.
I was hysterical, but I must have passed out after a while from the sheer shock of the pain because the next thing I remember was the intubation quickly being pulled out of my throat, the strings being cut after binding me to the bed even as my brother forced his way into the ICU. I felt like they were scampering to hide evidence of an ICU torture chamber before my brother and mother discovered how they’d restrained me.
Apparently, I was making such a scene in the ICU and as they did not know what to do with me they had called up my brother and mom to see if they could calm me down. The instant after they took out the intubation tube, I was complaining and crying that the pain was absolutely unbearable.
Now, mind you, I’ve been living with severe neuropathic pain for quite some time and have a pretty high pain threshold. So, for me to complain about pain I imagine it must have been pretty extreme.
Situation gets still worse …
My family asked what kind of pain drugs the hospital were administering to me through the IV and were astonished to discover that I was only being offered ibuprofen! Crazy I know … after spinal surgery only to be given ibuprofen?!?
My family, understandably outraged, demanded that they switch immediately to morphine to get the pain under some semblance of control.
Also, my brother insisted that I be moved out of the ICU and down to the seventh floor spinal cord injury unit to my room so that at least one immediate family member could stay with me round-the-clock over the next few days.
I can’t remember if it was a day or two or three, but the pain was definitely not abating and they were claiming to have been giving me 8 mg of morphine per hour. To put readers in the picture here, 8 mg of morphine per hour would have knocked me out or caused me to start hallucinating, so clearly we were missing something.
It was only after my brother Mattias leaned really hard on the staff that we discovered what was really going on with my medication. Chinese physicians generally have an aversion to the use of morphine, and sometimes they may also cut costs by diluting drugs. In any event, a junior nurse revealed to me in the middle of the night that, yes, the morphine being administered to me had been diluted.
All Hell broke loose again … Mattias was so angry he was intermittently speechless with rage, as he has opted to sleep with me and had thereby himself suffered a succession of sleepless nights as I moaned and screamed.
Perhaps fearing Mattias might assault a member of staff (I’ve ever seen my brother so angry) the medical team changed course and the morphine pump was suddenly filled with the real thing. But this was crazy, as the 8 mg/hour pump setting had not been reset.
So I started hallucinating and seeing spiders crawling down my wall in addition to the walls melting … and my blood oxygen saturation collapsed suddenly to 70% from a reference normal 98%, leaving me gasping for breath.
I do remember asking Mattias to make sure I didn’t get eaten by the spiders.
After a few days of back-and-forth we finally got the morphine dosing cut very sharply, but we overshot the mark and then the pain returned with a vengeance.
My Dad spoke urgently with surgeons in the United States and Australian, and finally an Australian military surgeon offered battlefield triage advice on how to use what medications we had on hand at the apartment for painkilling purposes. And they came up with a “cocktail” comprised of morphine sulfate and diazepam (Valium) that worked wonders.
After about seven days I was able to go home and rest for the next few weeks.
Truth be told, I remember the exact hours after the ICU very vividly, but much of the rest of the seven days in the hospital was a blur. I think my brain shut out much of that that experience because the pain levels were just intolerable.
I have to give all the credit to my family because they stayed up with me 24 hours a day, 7 days a week making sure that I survived this ordeal.
I have had several nightmare ICU experiences before this one, and I’ve a hunch that every SCI patient probably has an equally terrifying story, so we were prepared for almost every scenario except the one we encountered.
😦
So I turned out to have been the pioneer … the one with the arrows in her back!
But I’m past this now, being grateful simply to have survived and focusing on getting on with life and on my vision for how to put my uninjured brain to productive work as a professional trader.
Nonetheless, I encourage all hospital patients to question everything imaginable and try to assess independently what would be an acceptable standard of care. In my case, post-surgical ibuprophen didn’t cut it, and Tongren Hospital seems to have learned about as much as myself from my bizarre experience.
In conclusion, I will say that Tongren Hospital now administer much stronger pain meds to spinal surgery patients, and I have not heard of any more cases of nurses tying patients to hospital beds or diluting drugs.